If you’ve had unprotected sex or are worried about possible infection with Chlamydia or other STIs, get tested as soon as possible – even if you have no symptoms.
What is Chlamydia?
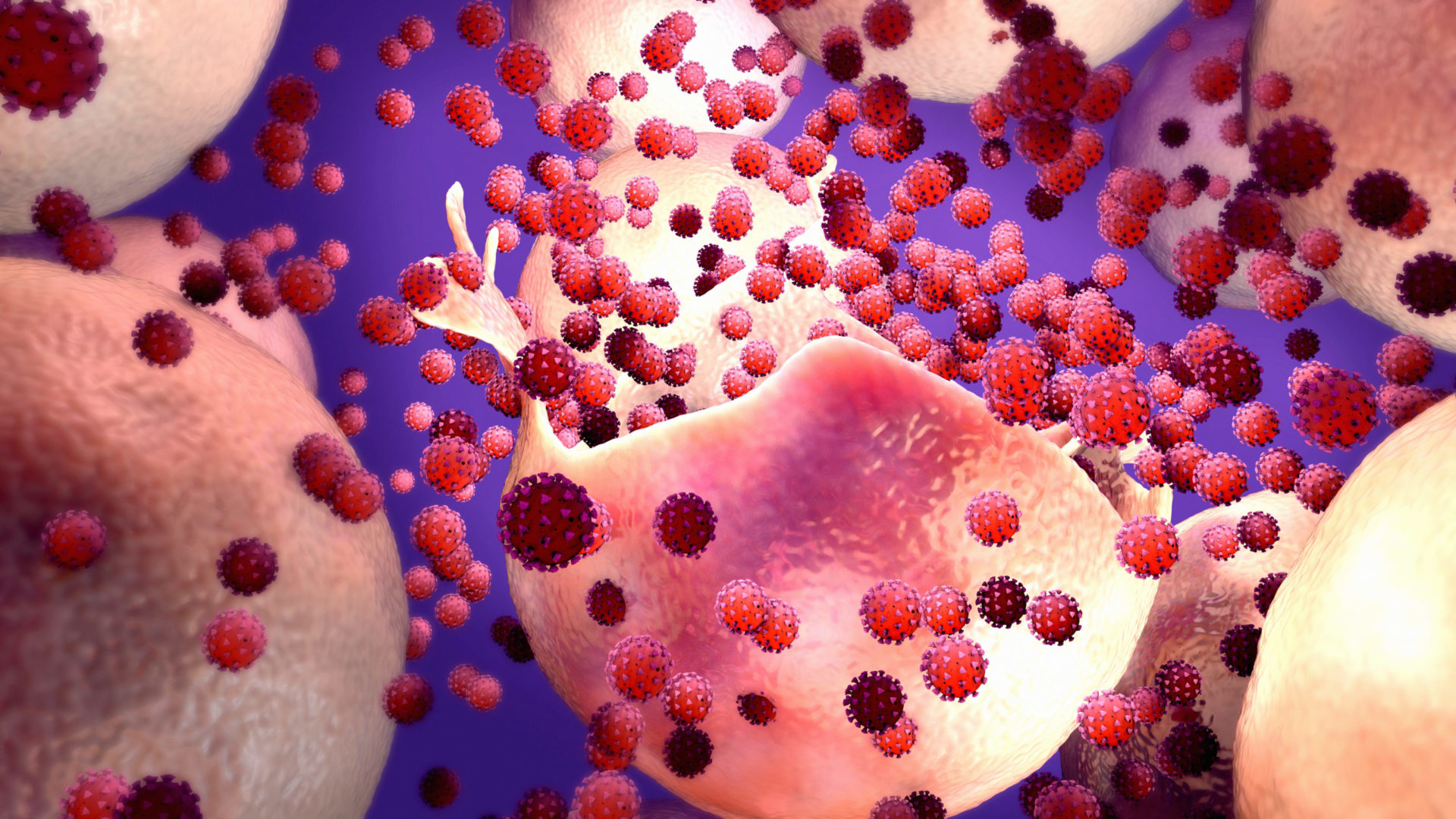
Chlamydia is a sexually transmitted infection caused by a bacterium called Chlamydia trachomatis.
Is Chlamydia a serious condition?
It usually causes no symptoms and can be easily treated with antibiotics. However, if not treated early, it can spread to other parts of the body and lead to long-term health problems.
How do I get Chlamydia?
Chlamydia can be transmitted very easily. You can get Chlamydia if:
- you have unprotected sex (sex without a condom or dental dam), vaginal, anal, and oral sex with someone who has Chlamydia (even if they have no symptoms);
- use sex toys that are not washed or covered with a new condom every time you use them;
- your genitals come into contact with your partner’s genitals – this means you can get Chlamydia from someone, even if there is no penetration, orgasm or ejaculation;
- you come into contact with an infected person’s semen or vaginal secretions, or if they get into your eyes.
Chlamydia, HIV and sexual health
- If you have an STI, including Chlamydia, your risk of getting HIV increases. This is because most STIs cause lesions that make it easier for HIV to enter the body.
- If you live with HIV and have Chlamydia, your viral load may be higher because your immune system is weaker. This will make you more likely to transmit HIV if you have sex without a condom.
- However, if you have an undetectable viral load (because you are taking the correct treatment for HIV infection), there is no evidence to show that Chlamydia infection increases your risk of transmitting HIV.
- If you are taking antiretrovirals, it is important to discuss with your doctor how treatment for Chlamydia might interact with ARV drugs.
How do I protect myself against Chlamydia?
- Use a new condom (male or female) or a dental dam every time you have anal, vaginal, or oral sex.
- Use a new dental dam or latex gloves for rimming and fingering (exploring your partner’s anus with your fingers, mouth, or tongue) or use latex gloves for fisting.
- Cover sex toys with a new condom and wash them after use.
- Limit the number of sexual partners you have, remember to use a new condom for each partner and get tested regularly.
Note – apart from condoms, other types of contraception (such as contraceptive pills) or PrEP do not protect against sexually transmitted infections.
What are the symptoms of Chlamydia infection?
Many people with Chlamydia have no symptoms. If you do have symptoms, you may not notice them until a few weeks after infection. In other cases, it may take up to several months or until the infection spreads to other parts of the body. You may also have a Chlamydia infection in your penis, anus, throat, or eyes.
Symptoms in men include:
- a white, cloudy or watery (colorless) discharge from the penis
- pain or burning when urinating
- pain and/or swelling of the testicles
- pain or bleeding from the anus (bottom).
Symptoms in women include:
- increased vaginal discharge caused by inflammation of the uterus in the cervical area
- pain or burning when urinating
- pain during sex and/or bleeding after sex
- pain in the lower abdomen – especially when having sex
- bleeding between periods and/or heavier, painful periods
- pain or bleeding from the anus (bottom).
Symptoms for both women and men include:
- inflammation (redness) of the eye (called conjunctivitis) caused by contact with semen or vaginal fluid (if it gets into the eye).
Can I get tested for Chlamydia?
Yes – medical staff may request a urine sample.
For men, a swab can be taken from the tip of the penis (urethra). If you have had anal or oral sex, a swab may need to be taken from your rectum (bottom) or throat. In some countries a self-collection kit is available.
If you have Chlamydia, you should also be tested for other STIs. It’s also important to tell your recent sexual partner so they can also be tested and treated. Many people who have Chlamydia don’t notice anything, and by telling them, you can help stop transmission and also prevent reinfection.
How is Chlamydia treated?
Chlamydia is easily treated with antibiotics.
Whether or not you have symptoms, don’t have sex until you and your partner have finished treatment. If you’ve had a one-day treatment, you should avoid sex for seven days after finishing treatment. Ask your doctor when it is safe to have sex again.
Note: – you can get Chlamydia even if you’ve had it before. Treatment cures the current infection but does not make you immune – this means you can get infected again.
Complications of Chlamydia infection
- As with most STIs, Chlamydia puts you at risk of getting other STIs, including HIV.
- Untreated, Chlamydia can lead to other health problems.
In men:
- Epididymitis – infection of the tubes that carry sperm from the testicles to the outside, which can cause fever, pain in the testicles and swelling.
- Urethritis – inflammation of the urethra (the tube that carries urine from the bladder out of the body).
- Prostatitis – infection of the prostate, which can cause pain during or after sex, fever and chills, painful urination, and lower back pain.
- Rarely, Chlamydia can cause infertility in men.
In women:
- Pelvic inflammatory disease (PID) – infection of the uterus, ovaries and fallopian tubes causing pelvic pain and fever. BIP can cause long-term pelvic pain, inability to get pregnant and potentially fatal ectopic pregnancy (pregnancy outside the womb). BIP can be treated with antibiotics.
- Cervicitis – inflammation of the lower part of the uterus (the cervix).
- Salpingitis – inflammation of the fallopian tubes (tubes that carry eggs from the ovaries to the uterus), preventing an egg from passing from the ovary to the uterus. This can be treated with surgery.
- Bartholinitis – swelling of the Bartholin’s glands – Chlamydia can cause blockage and infection of the glands that produce the lubricating mucus, leading to a cyst that can become infected and turn into an abscess. The abscess can be treated with antibiotics.
In both women and men:
- Reactive arthritis – inflammation of the joints and, in some people, the urethra and eyes (conjunctivitis). Pain pills can control symptoms.